Anthropologist, psychotherapist, and eating-disorder survivor Rebecca Lester shares the struggles of recovery, the failure of institutions—and a way forward.
Let’s start with some facts.
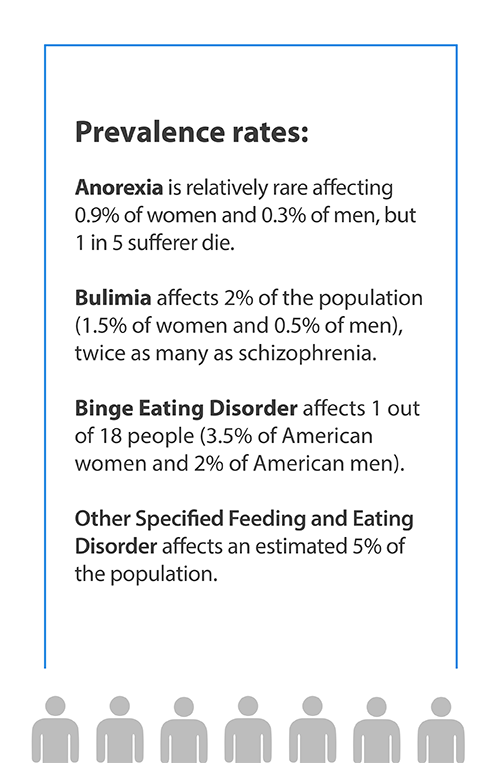
- Eating disorders affect an estimated 1 out of 7 people, making them more than five times as common as autism and more than ten times as common as schizophrenia.
- They are deadlier than breast cancer and affect more people per year than car accidents.
- Fewer than 1 in 10 people with an eating disorder will access mental health care, and only half will fully recover.
- 1 in 5 will remain ill or die.
With numbers as dismal as these, we have to ask: how did we get here?
 According to Rebecca Lester, associate professor of sociocultural anthropology at Washington University in St. Louis, misconceptions about eating disorders pervade not just public understanding, but the very institutions that are supposed to prevent and treat the conditions. And she should know. Diagnosed with anorexia for the first time at the age of 11, Lester has spent most of her life trying to figure out how to improve treatment and recovery rates.
According to Rebecca Lester, associate professor of sociocultural anthropology at Washington University in St. Louis, misconceptions about eating disorders pervade not just public understanding, but the very institutions that are supposed to prevent and treat the conditions. And she should know. Diagnosed with anorexia for the first time at the age of 11, Lester has spent most of her life trying to figure out how to improve treatment and recovery rates.
Her experiences in clinics—first as a patient, then as an anthropologist collecting ethnographic research, and finally, as a psychotherapist—have given her a multifaceted understanding of issues and challenges that surround eating disorders and recovery.
“Eating disorders are really misunderstood conditions,” Lester says. In order to improve treatment and save lives, she says, it’s time to confront and move on from these common misconceptions.
A Legacy of Mistrust and Misinformation
Traditionally, people assume that white, adolescent girls from middle- or upper-class families are those most at risk for developing eating disorders; however, Lester says this bias comes from the fact that much of the early research done on eating disorders relied on clinical populations—those already seeking treatment in private (read: expensive) clinics.
 “As people are doing more community-based studies, they’re realizing that this is a much more widespread problem than we thought,” Lester says. “Anyone can be at risk for developing an eating disorder—in different ways and for different reasons. You can’t rule anyone out for gender, race, or age.”
“As people are doing more community-based studies, they’re realizing that this is a much more widespread problem than we thought,” Lester says. “Anyone can be at risk for developing an eating disorder—in different ways and for different reasons. You can’t rule anyone out for gender, race, or age.”
Additionally, the Victorian predecessor of eating disorders skews the public and institutional understanding and sympathy towards eating disorders. “If you look historically, female hysteria got refracted into a number of different diagnoses, including eating disorders,” Lester says. “A lot of the old assumptions and ideas about hysteria, that this is a conflict about sexuality, or a desire to regress to childhood, or that it’s a way of manipulating other people, have also filtered in—even in the more biologically focused model that we have today.”
Because of the legacy of hysteria, Lester says, “there’s a kind of trivializing that often happens. Many people think ‘oh it’s a young, white, wealthy, teenage girl, who just wants to be beautiful and doesn’t eat so she can be thin.’ It’s hard to take eating disorders seriously if that’s your perspective. It’s totally erroneous, but it’s such an enduring set of ideas in our culture that it leads to dismissing what is a very serious condition.”
Misinformation, Institutionalized
Unfortunately, these prejudices seep into the very system that is supposed to support and care for those with eating disorders.
Eating disorders are the least covered psychiatric conditions in the American managed care heath insurance system. A 2015 study found that 21% of insurance plans categorically exclude eating disorders from coverage, compared with only 5.9% that excluded autism and 0% that excluded drug and alcohol treatment. Even under the Affordable Care Act, which says there must be parity with mental and physical illness, eating disorders are not technically qualified as a major mental illness.
“What are you going to do when your child is on death’s door? You’re going to get them treatment no matter what the cost.”
“Generally speaking, insurance companies really, really don’t like paying for eating disorder treatment,” Lester says. “It’s expensive. It requires a multidisciplinary team, including a psychiatrist, a medical doctor, and a dietician. So the right care is expensive, and relapse is high. It’s a reality. But as a result, a lot of insurance companies will exclude them altogether from coverage. Or they will authorize a short amount of time, which ends up cutting the treatment short and leads to relapse, and then that seems to justify the whole decision in the first place.”
The results can be devastating for those seeking treatment and their loved ones. “A number of families that I know have had to fight tooth and nail to get any kind of coverage, or they’ve gone bankrupt because they couldn’t get any financial help,” Lester says. “What are you going to do when your child is on death’s door? You’re going to get them treatment no matter what the cost.”
Despite the best intentions of care providers, they all too often become another cog in the wheel of relapse and recovery. “The clinicians I’ve worked with are extremely dedicated, and are working really hard to deliver care in a system that really makes it almost impossible to do that,” Lester says. “They’re being constantly evaluated and monitored by the insurance companies, who want to protect their investment. They want to see recovery. And if progress isn’t seen, or isn’t happening quickly enough, they can stop payment. It leaves very little room for somebody to struggle.”
The Necessity of Struggle—and Understanding
In order to improve the practices and policies of insurance companies and institutional care, Lester believes that a greater understanding of the disorders and the process of recovery is needed.
First, institutions must move beyond the legacy of female hysteria. Eating disorders are “really serious mental and physical disorders characterized by deep feelings of being out of control with one’s food and body,” Lester says. While food and eating patterns are at the heart of these conditions, they are emblematic of much deeper psychological and emotional issues.
“Eating disorders are not (and yet are) about food the same way rape is not (and yet is) about sex,” Lester writes. “Of course on the surface, it looks like it’s a struggle about food,” she says, “but if people take some time and talk to people who are struggling, then you realize really quickly that this is a much deeper, much darker and more difficult issue that’s going on.”
Lester has taken that time, spending countless hours listening to and counseling others with eating disorders. From 2002-2009, she conducted ethnographic research at a private eating disorder clinic in the Midwest that provided a variety of treatment programs for patients, ranging from 24-hour care to weekly outpatient therapy visits.
"On the surface, it looks like it’s a struggle about food, but if people take some time and talk to people who are struggling, then you realize really quickly that this is a much deeper, much darker and more difficult issue that’s going on.”
In addition to standard ethnographic activities like attending group therapy sessions and client meals, as well as interviewing patients, families, and staff, Lester completed her clinical practicum for her Master of Social Work degree at the recovery center. She also worked an additional 3,000 hours to become a fully licensed psychotherapist. In this capacity, she held individual therapy sessions with patients, charted client recovery and experiences, and coordinated with the other clinicians, patient families, and insurance companies.
From her own experience with recovery and from these innumerable testimonies, Lester says the issues underlying eating disorders often include larger themes like lacking a sense of agency in one’s own life, or may reflect the boundaries, or lack thereof, one maintains with others. These deeper issues vary from person to person and require the help of a trained therapist to work through.
When an eating disorder stems from these deeper issues about agency or boundaries, it would be normal—healthy even! Lester says—for a patient to rebel, to explore, to test their boundaries, especially in a safe environment. However, insurance companies often see a failure to comply with rules, or a refusal to eat, as a lack of commitment to recovery on the patient’s part.
Breaking Down Persistent Myths
Hear Rebecca Lester talk more about her research on the Arts & Sciences podcast series Hold That Thought.
“When that happens, the clinicians are in a place of trying to recognize as a therapist that this person is struggling and needs help,” Lester says, “but at the same time, having to represent to the insurance company that, no, they are actually still getting better.”
The true path to recovery is often much more winding and complex. “Just because you have two people with the same diagnosis of anorexia or bulimia, doesn’t mean they need the same kind of care,” Lester says. “Usually when people go to treatment, they’re in the worst place that they could be, emotionally and mentally. It’s incredibly challenging for people. So when they get really defensive in groups, or become highly critical, or isolate, or makes best friends with everybody, that becomes cues to the clinicians about maybe what larger issues that person is struggling with.”
Ideally, says Lester, insurance companies would follow the guidelines put forth by the American Psychiatric Association. “It’s more expensive in the short term to follow the guidelines,” she adds, “but it saves a lot of money in the long term when people aren’t going to the emergency room or relapsing back into the hospital, because they’ve actually gotten the care they need.”
A Way Forward: Compassion and Curiosity
“Even at 11, in the recovery center for the first time, I remember thinking ‘there has got to be a better way,’” Lester recalls. When a relapse with anorexia and bulimia at 18 sent her back to treatment, Lester began to consider not just her own recovery, but how she might help communicate what was going on for her and others like her to a system and caretakers who didn’t always understand.
“Obviously people who go into this line of work at the clinics are very well intentioned,” Lester says, “but that still doesn’t mean that you really understand or that you have the tools that you need. As I went through college and into graduate school, I decided it was really something I wanted to focus on. And that was a big motivator for me and my own recovery and getting well. That if I wanted to help other people, I had to do the work myself, and be well enough to do that.”
“People can get well. I’ve seen it happen. It’s not an easy thing, and it’s not a decision that people make like, ‘Oh, I decided to get well.’ It doesn’t work like that. But it’s possible.”
Now, she has three different lenses through which to view, understand, and communicate the struggles associated with eating disorders: anthropology, psychotherapy, and as a person in recovery. She credits her anthropology training with helping her take someone else’s perspective in the clinic, to see the world from their point of view, and to help understand how they give meaning to things that are unique and individual.
 Meanwhile, her own life experiences make the work extremely personal. “It’s who I am,” she says. “It animates my work because I have such strong feelings about it—both about how serious these conditions are and how trivialized they tend to be. But also, the hope that I have and the really strong belief I have that people can get well. I’ve seen it happen. It’s not an easy thing, and it’s not a decision that people make like, ‘Oh, I decided to get well.’ It doesn’t work like that. But it’s possible.”
Meanwhile, her own life experiences make the work extremely personal. “It’s who I am,” she says. “It animates my work because I have such strong feelings about it—both about how serious these conditions are and how trivialized they tend to be. But also, the hope that I have and the really strong belief I have that people can get well. I’ve seen it happen. It’s not an easy thing, and it’s not a decision that people make like, ‘Oh, I decided to get well.’ It doesn’t work like that. But it’s possible.”
And Lester truly has dedicated her life to this cause. Currently, in addition to her position at WashU, Lester runs a small private practice to continue to treat those with eating disorders and related issues. She notes that her practice is a nonprofit and does not take any money from insurance companies. She’s also working on a book manuscript, based on her ethnographic work at the clinic and her practice as a psychotherapist, that provides both a critical and constructive perspective on eating disorders and eating disorders treatment in the era of managed care.
For those out there wondering what to take away from all of this, Lester gives two words advice: “Compassion and curiosity.”
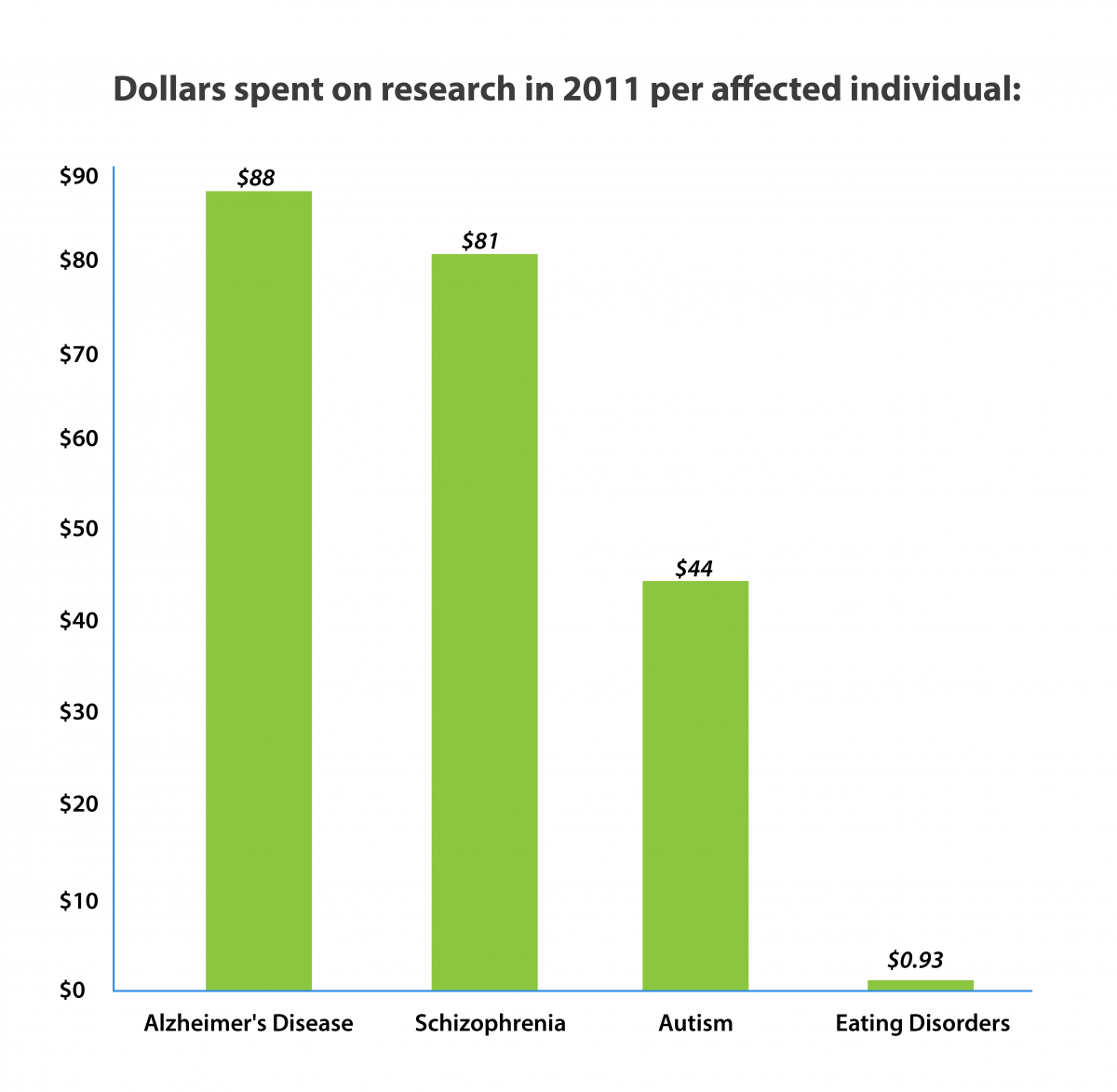
“It can be really difficult to interact with someone in the throes of an eating disorder,” she says. “People get mean—I mean, they’re starving. They’re struggling. I think I would want people to have a deeper compassion for the seriousness of what these conditions are, and a curiosity to really want to learn about them. The kinds of mobilizing around autism and breast cancer, we need the same kind of mobilizing around this issue. I think that will make people more invested, so that others can get treatment.”





