Funding from the National Institutes of Health will help Jackrel and her team study Matrin-3, a poorly understood protein linked to several neurodegenerative disorders.
The relentless neurological disease amyotrophic lateral sclerosis (ALS) eventually shuts down the entire body, but the devastation starts at a molecular level. Over the years, researchers have linked ALS, also called Lou Gehrig’s disease, to a handful of proteins that don’t function properly because of genetic mutations. Over time, these distorted or “misfolded” proteins can clump together in the brain and nervous system, potentially gumming up normal nerve function and starting the slow march to total paralysis. In theory, it might be possible to stop the disease by repairing and preserving these proteins—a possibility that has inspired ongoing experiments and tantalizing findings in the lab of Meredith Jackrel, assistant professor of chemistry.
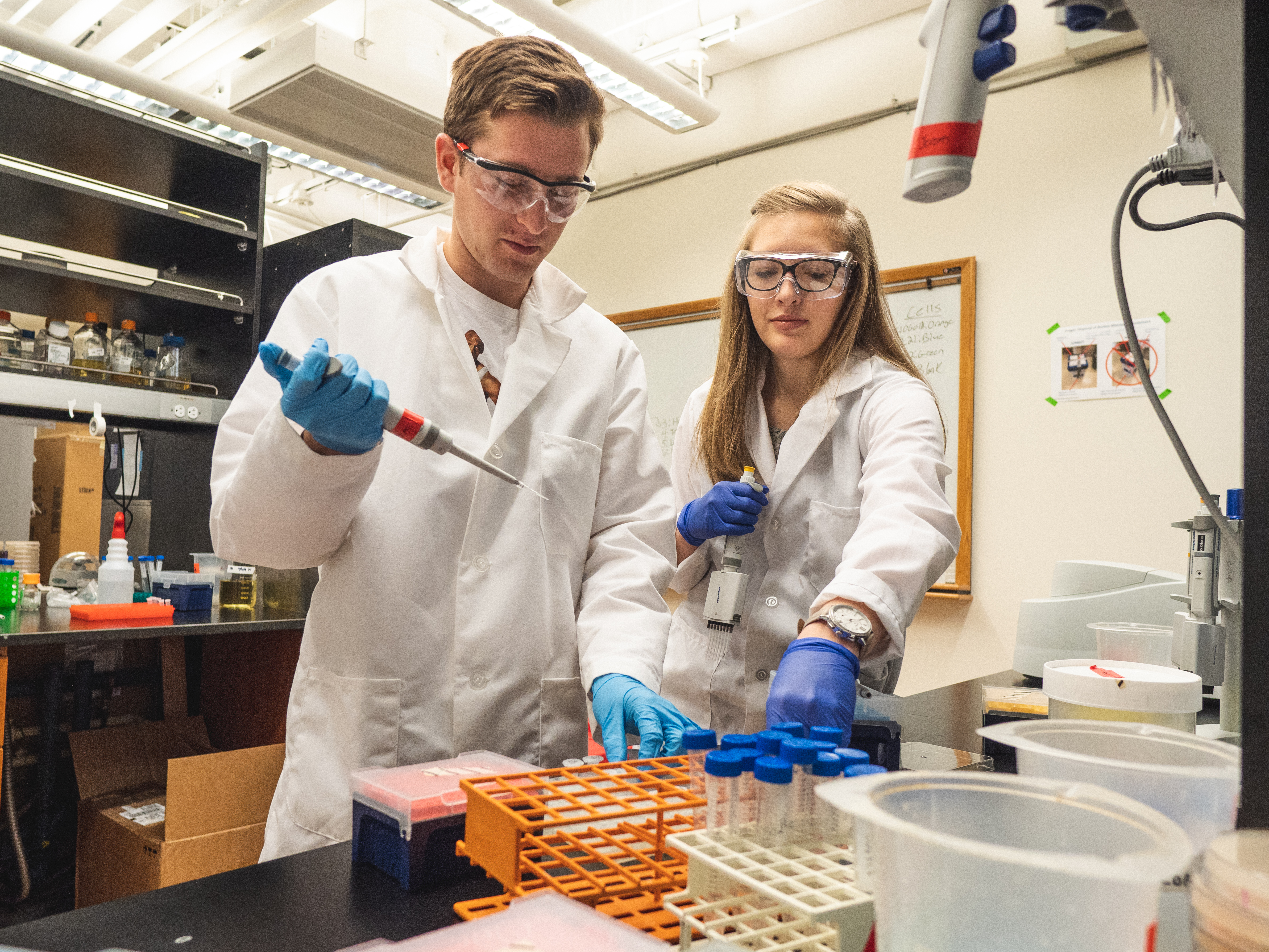
Neurological diseases may seem like an unusual area of research for a chemist, but Jackrel’s expertise with the structure and function of proteins has put her in position to make real progress against ALS. Last month she received a grant from the National Institutes of Health (NIH) worth nearly $430,000 to further her research into Matrin-3, a poorly understood protein that appears to play a pivotal role in some cases of ALS and frontotemporal dementia (FTD), a type of dementia caused by damage to the neurons in the frontal and temporal lobes of the brain. “There have been very few papers on Matrin-3,” Jackrel said. “It’s been very understudied. We want to understand its intrinsic properties and how it might be disrupted in ALS and FTD."
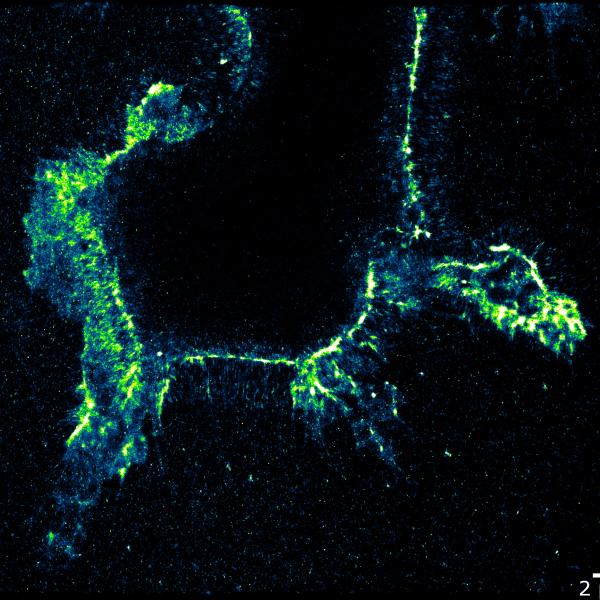
The grant will help Jackrel build on previous work that suggests a potential way forward in the fight against ALS. In a March 2022 paper published in the journal iScience, she and her team developed a new system to study Matrin-3 in yeast, an organism that naturally produces many of the same proteins found in humans. Experiments showed that clumps of misfolded Matrin-3 were toxic to yeast, and using this system they uncovered several key features that dictate how Matrin-3 functions and how genetic mutations can disrupt these functions. They also went on to show that engineered variants of the enzyme Hsp104 can successfully reverse the misfolding and break up the clumps, rendering the proteins harmless to the growing yeast. The results suggest that the fundamental underpinnings for ALS might be reversible, a tantalizing prospect that warrants much further investigation. “We’re very excited about the possibilities,” Jackrel said.
Jackrel explains that misfolding of Matrin-3 and similar proteins likely causes trouble in two ways: Not only do the clumps of distorted proteins disrupt processes within cells, but the proteins also no longer serve their normal jobs. “Matrin-3 is known to have a lot of important functions,” Jackrel said. For example, it’s abundant in the matrix that surrounds the genetic material in the nucleus inside of cells, making it potentially important for the proper function and integrity of the cell. It also binds the messenger molecule RNA, which means it likely plays a role in gene expression. Misfolding makes all of these jobs difficult if not impossible. “There seems to be a toxic loss of function,” she said.
With this new NIH funding, Jackrel and her team will explore how Matrin-3 compares to other proteins that are associated with ALS and FTD. Jackrel explained that a large percentage of patients with ALS have mutations in the gene for a protein called TDP-43. “Matrin-3 and TDP-3 seem very similar to each other, but they have different RNA binding properties,” Jackrel said. “We really want to understand how those proteins are similar, how they are different, and how that might drive ALS,” she said.
She is also planning to continue working on fine-tuning the engineering of her Hsp104 enzymes. The enzymes that showed such promise for repairing Matrin-3 in the 2022 paper were identical to enzymes used in previous experiments with TDP-43. “We didn’t tailor the enzyme to Matrin-3,” she said. Further tweaks to specifically target Matrin-3 might significantly increase the efficiency and potency of the enzyme.
Jackrel hopes her work will help point the way toward a successful strategy for eventually treating or preventing ALS, FTD, and related neurodegenerative diseases, but such an advance is, at best, still far in the future. At this time, it’s not certain that dissolving the clumps of misfolded proteins or preventing the misfolding in the first place will actually slow the disease. “We don’t know what the therapeutic goal should be,” she said. Even if HSP104 or similar enzymes don’t prove useful against the disease, she anticipates that experiments like hers will lay the groundwork for further investigations of other potential therapies. In particular, she believes that the yeast model used in her lab could become a useful platform to test a wide variety of other approaches.
Because Jackrel’s projects span the disciplines of chemistry and medicine, she often collaborates and consults with researchers at Washington University School of Medicine. “We interact with researchers at the medical school quite frequently,” she said. One of those collaborators is Gus Davis, MD, PhD, an assistant professor of neurology who sees much promise in Jackrel’s approach. “Dr. Jackrel’s work has great potential to increase our understanding of the fundamental biochemistry of protein misfolding in the context of neurologic disease and should help to pave the way for novel therapies,” Davis said.